I. Introduction
In 2017 the CDC reported more than 2.8 million total deaths due to various causes [1]. Diseases of the heart were the number one cause of death with a count of more than 647,000. Influenza and pneumonia caused more than 55,000 deaths and were ranked 8th in causes of death. By August 20, 2020, the US has seen more than 175,000 deaths due to COVID-19. Charbel el Bcheraoui et al. documented a declining trend of infectious disease mortality in the US due to better health care and vaccines from 1980 to 2014. They however did conclude that infectious diseases do pose a major health threat due to an increase in contact between humans and previously unknown pathogens [2]. Ethnicity combines the effects of a person’s genetic make-up, social constructs, including cultural identity, and also behavioral patterns [3]. Ethnicity could likely contribute to the spread of the virus in a community; for example, cultural, behavioral, work and living differences due to lower socioeconomic status, health-seeking behavior, and intergenerational cohabitation seen in certain communities could all contribute. So far, none of the top ten countries with COVID-19 cases have reported ethnicity-related data. In the UK, mortality reporting does not require documentation of ethnicity-related information. Understanding the relative importance of ethnicity-related factors will require both qualitative (behavioral response to pandemic) and quantitative (absolute risks and outcomes) prospective studies [4].
Rentsch et al. [5] study analyzed about 6 million US veterans to understand racial and ethnic disparities in COVID-19 testing and subsequent mortality. The study found that both African Americans and Hispanics were more likely to be tested for COVID-19 and both groups tested positive for the infection at a higher rate than Caucasians. These findings were true irrespective of an individual’s underlying health conditions, age, gender demographics, and geographical location. However, this study did not find a difference in 30 day mortality when comparing between race or ethnicity [5]. Multiple studies of large US metropolitan areas (e.g. Chicago, Illinois and Milwaukee County, Wisconsin), with higher concentrations of racial and ethnic minorities and adverse social determinants that may not adequately permit safe social distancing, have been conducted. These studies have shown a higher rate of COVID-19 infections in these areas. Gaining a better understanding of COVID-19 infections related to various demographic factors is necessary to come up with better healthcare services for minority populations [6,7]. This paper specifically looks at demographic factors such as age, race, gender, and state of residence to find out which demographic factors contribute most to COVID-19 deaths in the United States. This comprehensive analysis is conducted over the first eight months of 2020 using two different CDC-based data sets. Furthermore, a novel Qualitative socio-economic Logic based Cascade Hypotheses (QLCH) of education, occupation, and income affecting race/ethnicity are evaluated using US government’s latest socio-economic data reports. A better understanding of how these demographic factors in concert with socio-economic factors contribute to COVID-19 deaths will guide us in developing better public policies to combat the pandemic.
II. Data acquisition and analysis
- Database selection
We used data collected by the CDC for both analyses, limiting our dataset to COVID-19 deaths for the first eight months of 2020 [8,9]. The first data set looked at several demographic factors including 11 age groups, race, and states of residence in respect to COVID-19 deaths for a total of 4,752 observations. The CDC uses the following race categorizes to organize COVID-19 related deaths: Hispanic, White, Black or African American, American Indian or Alaska Native, Asian, Native Hawaiian or Pacific Islander, and More than One Race. We could not make any conclusions concerning gender and COVID-19 deaths from the first data set as gender information was not included [8]. We excluded 89 observations from our analysis, as 88 observations were totals for the United States and one observation had a missing field. We turned again to the CDC for our second analysis because the first CDC data set, while providing information for age, race, and state of residence, did not provide information based on gender [9]. This dataset also covered the time frame for the first eight months of 2020. Out of 1,378 observations within the second data set, 212 observations were excluded from our analysis. These 212 observations included state totals for all genders-all ages, total for male-all ages, total for female-all ages, and total for unknown gender-all ages. - Hypothesis testing
Statistical analyses were performed with both data sets. We utilized a testing model with dependent variable y and independent variable xi, where i = 1, 2,…(1)
The hypothesis used for our model:
(2)
(3)
- Data analysis
- First analysis model
A visual display of the first CDC-based dataset is provided in Figures 1 through 3 for our first analysis model. These scatterplots show variations between race and deaths, age groups and deaths, and state and deaths. Figure 1 demonstrates that Caucasians have experienced more variation of deaths followed by African Americans, Hispanics, and then Asians. The other races have seen relatively fewer deaths.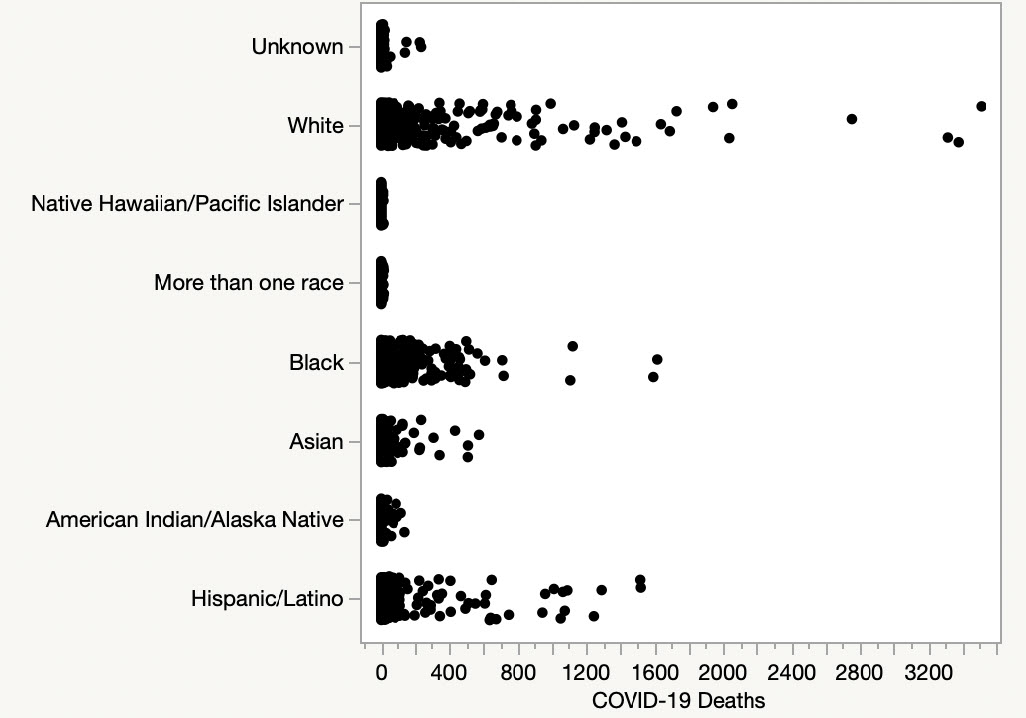 Figure 1: Race and deaths scatterplot
Figure 1: Race and deaths scatterplotFigure 1 confirms what Vahidy et. al [6] and Millett et. al [7] concluded in their paper: African Americans and Hispanics experienced a relatively higher proportion of deaths in reference to their respective population proportions. Figure 2 demonstrates an increase in the number of deaths as a function of age. Based off of the data, those individuals below the age of 55 have a relatively smaller chance of death from COVID-19 compared to those in age groups of 55 and above.
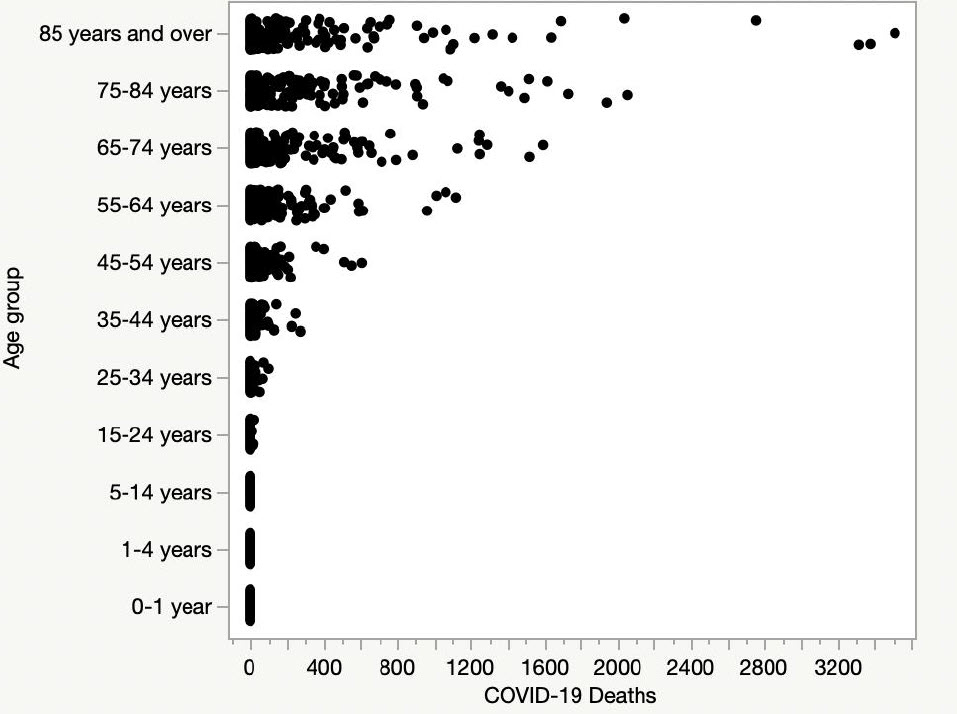
Figure 2: Age group and deaths scatterplot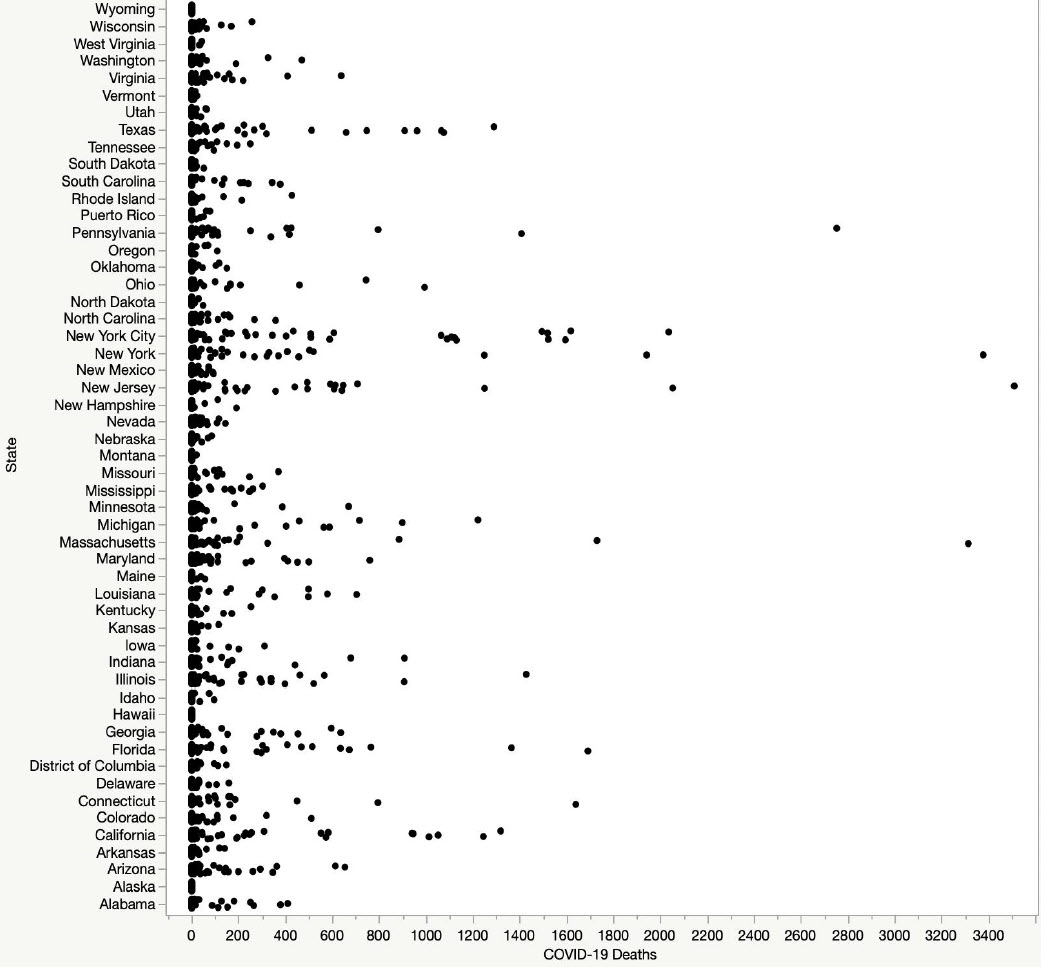
Figure 3: States and deaths scatterplotLastly, seven states (New Jersey, New York, Michigan, Pennsylvania, Florida, California, and Texas) were found to have a large variation in deaths compared to the other 43 states in the country, as displayed in Figure 3.
Using JMP software, we performed a multiple linear regression analysis. Our model’s summary of fit demonstrated an R-squared adjusted value of 0.2884. The analysis of variance of the full model is shown in Table 1. Our overall model was shown to be significant with a p-value of < 0.0001. This means that our regression model is better than just using a mean value to predict deaths. Table 2 shows that all individual
sources of state, race, and age groups are significant with COVID-19 deaths as each has a p-value < 0.0001. The parameter estimates for the first model are tabulated in Appendix A. Analyzing Appendix A for the pvalues (last column of ‘prob > |t|’), we can conclude that all age groups are significant to the regression model. In addition, all races are significant to the regression model, with the exception of African Americans
with a p-value > 0.05. Only a few states are significant to the regression model (California, Florida, Illinois, New York, Ohio, Pennsylvania, and Texas) with p-value < 0.05. All the remaining states are not significant to the regression model with p-value > 0.05.Table 1: ANOVA table – 1st data set
Source DF Sum of Squares Mean Square F Ratio Model 69 3977597530 57646341 19.4363 Error 3069 9102394794 2965915.5 Prob>F C. Total 3138 53345747 <0.0001
Table 2: Effect tests – 1st data set
Source DF Sum of Squares F Ratio Prob>F State 52 712786798 4.6217 <0.0001 Race 7 2149564759 103.5366 <0.0001 Age Group 10 1095127346 36.9238 <0.0001 Figure 4 shows the normalized residuals vs. predicted deaths for the first CDC data set-based model. There are many outliers, as several of the points do not fall within a -3 to +3 range for predicted deaths higher than 3,000.
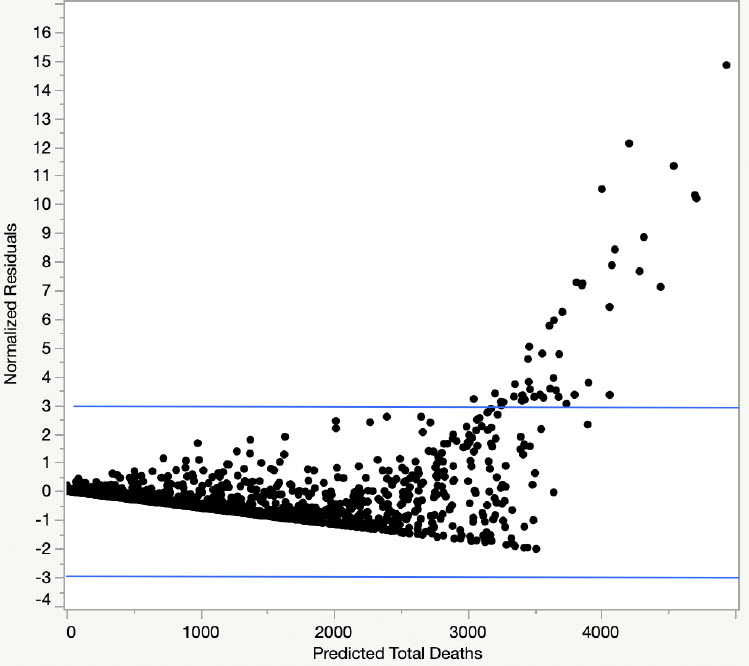
Figure 4: Normalized residuals plot - Second analysis model
For our second model, multiple regressions were performed using the second CDC data set. This model included age groups, gender, and state of residence with respect to COVID-19 deaths. A visual display of our CDC-based second dataset is provided in Figures 5 through 7 for this analysis model. These scatterplots show variations between age groups and deaths, gender and deaths, and state of residence and deaths. Figure 5 demonstrates that both males and females experienced a similar variation in deaths.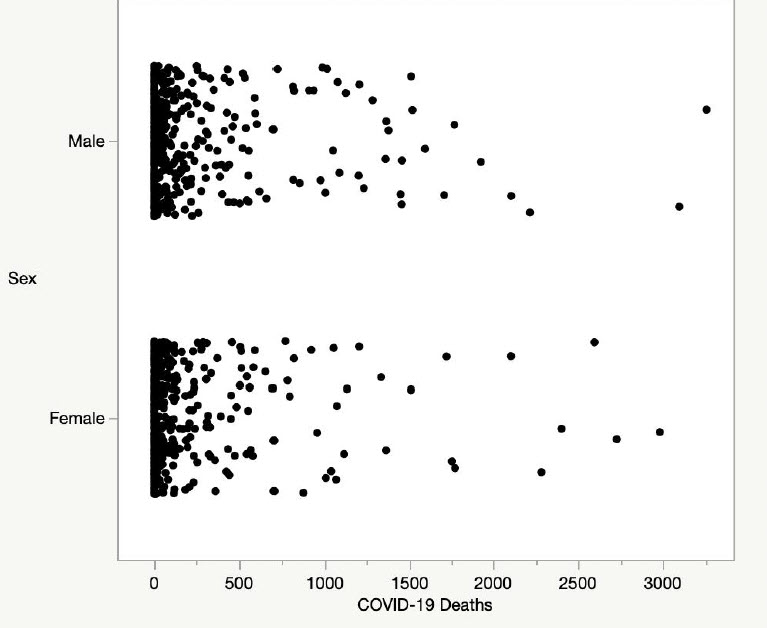 Figure 5: Gender and deaths scatterplotFigure 6 demonstrates an increase in the number of deaths as a function of age similar to the first data set shown in Figure 2. We reached the same conclusion that those individuals below the age of 55 have a relatively smaller chance of death in comparison to age groups of 55 and above.
Figure 5: Gender and deaths scatterplotFigure 6 demonstrates an increase in the number of deaths as a function of age similar to the first data set shown in Figure 2. We reached the same conclusion that those individuals below the age of 55 have a relatively smaller chance of death in comparison to age groups of 55 and above.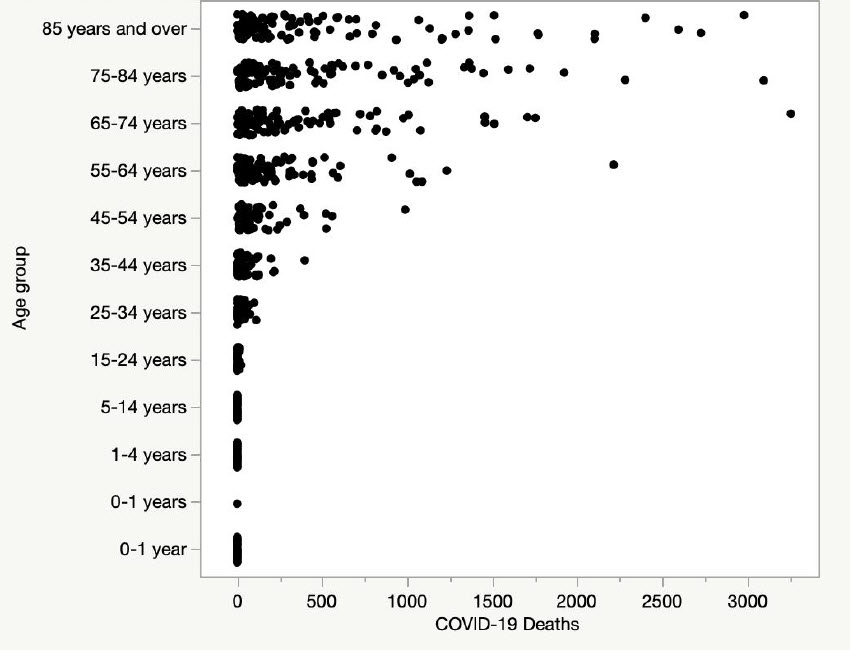 Figure 6: Age groups and deaths scatterplotFrom Figure 7, similar to Figure 3, seven states (New Jersey, New York, Michigan, Pennsylvania, Florida, California, and Texas) have a large variation in deaths compared to the other 43 states.
Figure 6: Age groups and deaths scatterplotFrom Figure 7, similar to Figure 3, seven states (New Jersey, New York, Michigan, Pennsylvania, Florida, California, and Texas) have a large variation in deaths compared to the other 43 states.
Table 3 shows the analysis of variance for the overall regression model for our second CDC data set. This was found to be significant with a p-value of <0.0001.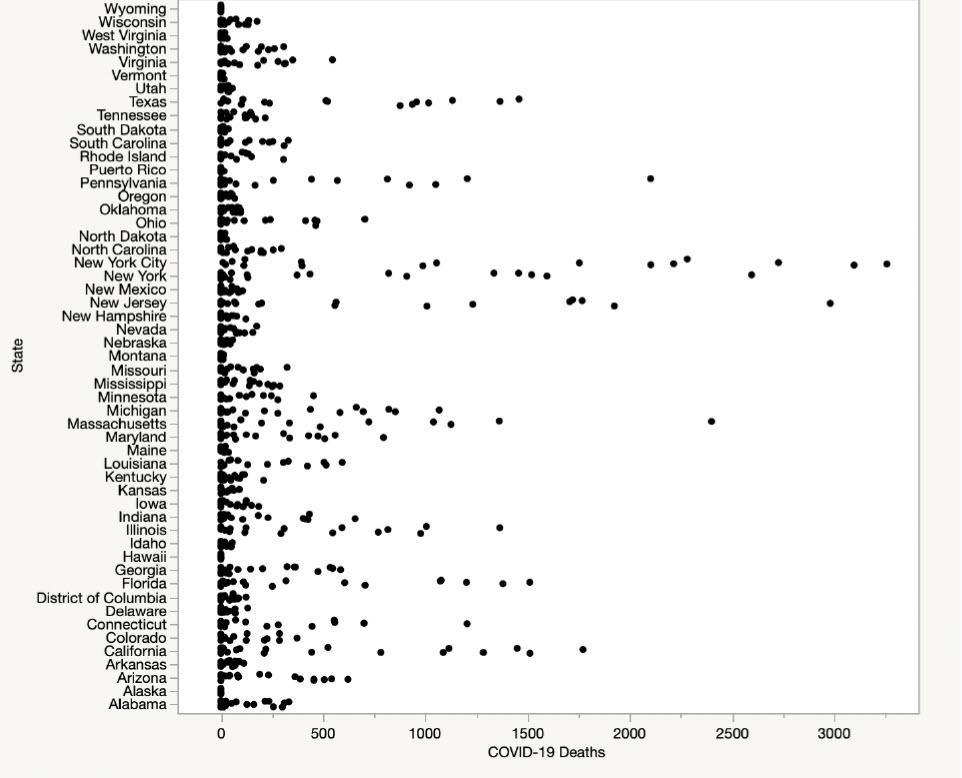
Figure 7: States and deaths scatterplotThese results show that our regression model is better than just using a mean value to predict deaths. The model had a R-squared adjusted value of 0.5437, thus displaying a better fit than our first model. Table 4 for this analysis demonstrates that age groups and states of residence are statistically significant (p-value < 0.05), while gender is not. Parameter estimates are tabulated in Appendix B. Analyzing Appendix B for the p-values (last column of ‘prob > |t|’) we can conclude that all age groups are significant to the regression model except the age groups of 1-4 years and 55-64 years as they both have p-value > 0.05. Unlike our first model, in this model most states that are significant to the regression model with p-value < 0.05. The states of Georgia, Hawaii, Indiana, Louisiana, Maine, Maryland, Minnesota, Mississippi, Missouri, Montana, North Carolina, Ohio, South Carolina, Tennessee, Vermont, Virginia, and Washington are not significant to the regression model with p-value >0.05.Table 3: ANOVA table – 2nd data setSource DF Sum of Squares Mean Square F Ratio Model 64 81481251 1273145 17.6413 Error 830 59899942 72169 Prob>F C. Total 894 141381193 <0.0001
Table 4: Effect tests – 2nd data setSource DF Sum of Squares F Ratio Prob>F Age group 11 32720764 41.22 <0.0001 State 52 49309527 13.14 <0.0001 Sex/Gender 1 254763 3.53 0.0606 In Figure 8 we show the normalized residuals vs. predicted deaths for the second CDC data set. There are no outliers, as none fall outside the -3 to +3 range.
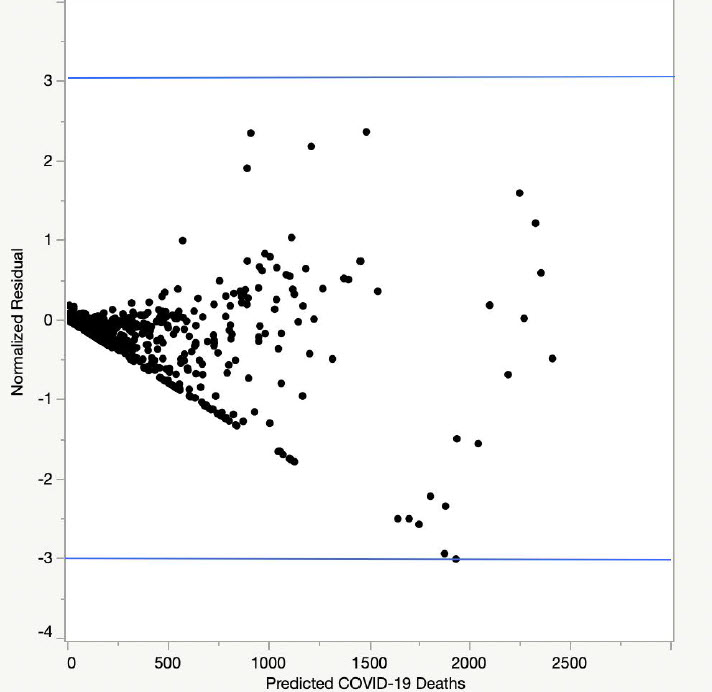
Figure 8: Normalized residuals plot
- First analysis model
III. Social Implications
- Socio-economic drivers
First, we propose Qualitative socio-economic Logic based Cascade Hypotheses (QLCH) related to education, occupation, and income. Second, we extend these four socio-economic hypotheses to ‘COVID-19 deaths related to race’ hypotheses. We next look at various US government’s socio-economic data of education, occupation, income, and where a person lived in reference to race/ethnicity to validate these hypotheses.- Qualitative socio-economic Logic based Cascade Hypotheses (QLCH) for a race
We propose the following Qualitative socio-economic Logic based Cascade Hypotheses:
QLCH1: A race with lower Highschool dropouts and higher Highschool completions will have higher college enrollments and college education completions and vice versa.
QLCH2: A race with higher college enrollment will have higher Bachelor’s degrees awarded in STEM (Science, Technology, Engineering, and Mathematics) fields and vice versa.
QLCH3: A race with higher numbers of Bachelor’s degrees awarded in STEM fields will have higher proportions of Management/professional jobs instead of Service jobs (including essential work of hospitals/transportation/farm/grocery stores jobs) and vice versa.
QLCH4: A race with a higher proportion of Management/professional jobs instead of Service jobs (including essential work of hospitals/transportation/farm/grocery stores jobs) will earn higher median incomes and vice versa. - Qualitative socio-economic Logic based Cascade Hypotheses (QLCH) to COVID-19 for a race
Next, we extend the four socio-economic hypotheses (QLCH1-4) to ‘COVID-19 deaths related to race’ hypotheses as follows:
QLCH5: A race with higher median incomes will have higher percentage of private health coverage and vice versa.
QLCH6: A race with higher proportions of Management/professional jobs instead of Service jobs (including essential work of hospitals/transportation/farm/grocery stores jobs) have a better capacity to social distance by working from home and vice versa.
QLCH7: A race with higher proportions of Management/professional jobs instead of Service jobs (including essential work of hospitals/transportation/farm/grocery stores jobs) have a better capacity to social distance by living in non-crowded neighborhoods like suburbs instead of cities and vice versa.
QLCH8: A race with higher proportions of living in non-crowded neighborhoods like suburbs instead of cities will have better healthcare access and vice versa.
- Qualitative socio-economic Logic based Cascade Hypotheses (QLCH) for a race
- Socio-economic data for the U.S.
In Tables 5 through 9 we display socio-economic data from various U.S. Government reports. Then for each table we verify if the data follows our various hypotheses.
In Table 5 we summarize data from the U.S. Department of Education’s National Center for Education Statistics for 2016 [10]. Asians performed the best in all categories with lowest Highschool dropout rate of 2%, highest Highschool completion rate of 97% and highest full time job holders of 80%, highest college enrollment rate of 58%, and highest Bachelor’s degrees awarded in STEM (Science, Technology, Engineering, and Mathematics) fields of 33%. Both Blacks and Hispanics were the bottom two races when it came to Highschool graduations, college enrollments, and receiving Bachelor’s degrees in STEM fields.Table 5: Graduation and jobs percentages by race in the US – 2016White Black Asian Hispanic Highschool dropout rate 5% 6% 2% 9% Highschool completion rate 94% 92% 97% 89% Highschool dropouts who are full time job holders 58% 39% 78% 65% Highschool graduates who are full time job holders 68% 66% 80% 72% College enrollment rate 42% 36% 58% 39% Bachelor’s degrees awarded in STEM* fields 18% 12% 33% 15% *STEM: Science, Technology, Engineering, and Mathematics
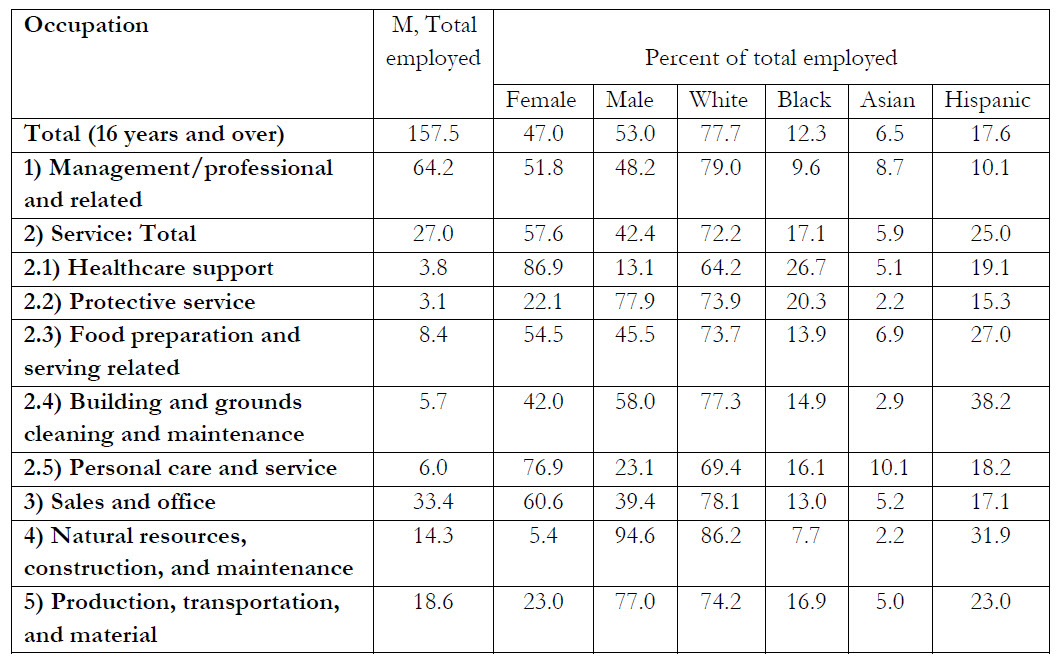
The QLCH1 and QLCH2 appear to apply well as shown in Table 5 to all four races and profoundly to Asians with lower Highschool dropouts, higher Highschool graduations, higher college enrollments, and higher Bachelor’s STEM degrees awarded. In Table 6, we display employment by occupation, gender, and race from the U.S. Bureau of labor statistics report for 2019 [11]. Note that the estimates for the race groups do not sum to totals, as data are not presented for all races and those people whose race is identified as Hispanic may be of any race. Both Asians and Whites hold proportionally more Management or Professional jobs than their population proportions (8.7% vs. 6.5% for Asians and 79% vs. 77.7% for Whites) while both Blacks and Hispanics hold proportionally fewer Management or Professional jobs than their population proportions (9.6% vs. 12.3% for Blacks and 10.1% vs. 17.6% for Hispanics). The opposite is true for ‘Service’ occupation as both Blacks and Hispanics hold proportionally higher Service jobs than their population proportions (17.1% vs. 12.3% for Blacks and 25% vs. 17.6% for Hispanics) while both Asians and Whites hold proportionally fewer Service jobs than their population proportions (5.9% vs. 6.5% for Asians and 72.2% vs. 77.7% for Whites). For the ‘Sales and office’ occupation, only Asians have lower proportional employment than their population proportion (5.2% vs. 6.5%) while the other three races’ proportional employments represent their individual population proportions. For the occupations of Natural resources, construction, and maintenance, Whites and Hispanics overrepresent while Blacks and Asians underrepresent their individual population proportions. For the occupations of Production, transportation, and material, Blacks and Hispanics overrepresent while Whites and Asians underrepresent their population proportions.
Thus, the data in Table 6 shows that all races do follow QCH3. Asians and Whites with higher percentage of STEM degrees hold higher proportions of Management/professional jobs and lower proportions of Service jobs (including essential work of hospitals/transportation/farm/grocery stores jobs) while Blacks and Hispanics with lower percentage of STEM degrees hold lower proportions of Management/professional jobs and higher proportions of Service jobs as compared to their respective population proportions.
Table 6: U.S. Bureau of labor statistics – 2019
In Table 7, we display health insurance coverage by race in the United States for 2018 from the census report [12]. Note that Hispanic data may overlap with data for race groups as Hispanics can be of any race. Both Whites and Asians have higher health care coverage percentages (94.6% and 93.2% respectively) including higher private insurance coverage (74.8% and 73.1% respectively). In contrast, both Blacks and Hispanics have lower health care coverage percentages (90.3% and 82.2% respectively) including significantly lower private insurance coverage (55.4% and 49.6% respectively). Relatively speaking, both Blacks and Hispanics have considerably higher public insurance coverage (41.2% and 36.5% respectively) than both White and Asians (33.2% and 26.1%)
For all four races QLCH5 applies well as described in Table 7. Asians and Whites with higher median incomes have higher percentage of private health coverage while Blacks and Hispanics with lower median incomes have lower percentage of private health coverage or higher percentage of public health coverage.Table 7: Health Insurance Coverage in the United States – 2018
Coverage White Black Asian Hispanic Health insurance coverage 94.6% 90.3% 93.2% 82.2% Private insurance coverage 74.8% 55.4% 73.1% 49.6% Public insurance coverage 33.2% 41.2% 26.1% 36.5%
Table 8: Life expectancy by race – 2017Age (Life expectancy in years) All races White Black Hispanic At birth 78.6 78.5 74.9 81.8 At age of 55 years 27.4 27.3 25.2 29.8 In Table 8, we show CDC’s life expectancy data by race at birth and at age of 55 years for 2017 [13]. Blacks had the lowest life expectancy both at birth and at age of 55 (74.9 and 25.2 respectively), while Hispanics had the highest life expectancy (81.8 and 29.8 respectively).
In Table 9 we display real median household income from the U.S. Census Bureau’s Current Population Survey [14]. Asians had the highest median income of 68,200,
68,200,  40,300 respectively. Blacks faired the worst with no real median income growth from 2002 to 2017 while Asians had the highest growth gains of 0.82% annually over the same period.
40,300 respectively. Blacks faired the worst with no real median income growth from 2002 to 2017 while Asians had the highest growth gains of 0.82% annually over the same period.Table 9: Real median household income by race in 2017 dollars
Year All races White Black Asian Hispanic 2017  68,200
68,200 81,400
81,400 58,000
58,000 40,300
40,300 45,000
45,0001987  57,500
57,500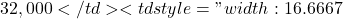 67,000
67,000$40,000 2002-2017 Annual Growth 0.38% 0.37% 0.00% 0.82% 0.77%
Table 10: Real median household income relative to Asian raceYear All races White Black Asian Hispanic 2017 0.75 0.84 0.50 1.00 0.62 2002 0.81 0.90 0.56 1.00 0.63 1987 0.79 0.86 0.48 1.00 0.60 Average 0.78 0.87 0.51 1.00 0.62 From Table 9, we converted real median household income standardized in terms of Asian median income which is shown in Table 10. Over a 30 year period from 1987 to 2017, Blacks made 51 cents on a dollar, Hispanics made 62 cents on a dollar, and Whites made 87 cents on a dollar when compared to Asians. Thus, the data shows that QLCH4 applies well to all four races as described in Table 9 and Table 10. Asians and Whites with a higher proportion of Management/professional jobs instead of Service jobs (including essential work of hospitals/transportation/farm/grocery stores jobs) earn higher median incomes, while Blacks and Hispanics with a lower proportion of Management/professional jobs instead of Service jobs (including essential work of hospitals/transportation/farm/grocery stores jobs) earn lower median incomes.
- Socio-economic implications of race and location of living to COVID-19
Applying QLCH6, Asians and Whites with higher proportions of Management/professional jobs instead of Service jobs (including essential work of hospitals/transportation/farm/grocery stores jobs) do have better capacity to social distance by working from home while the opposite will be true for Blacks and Hispanics.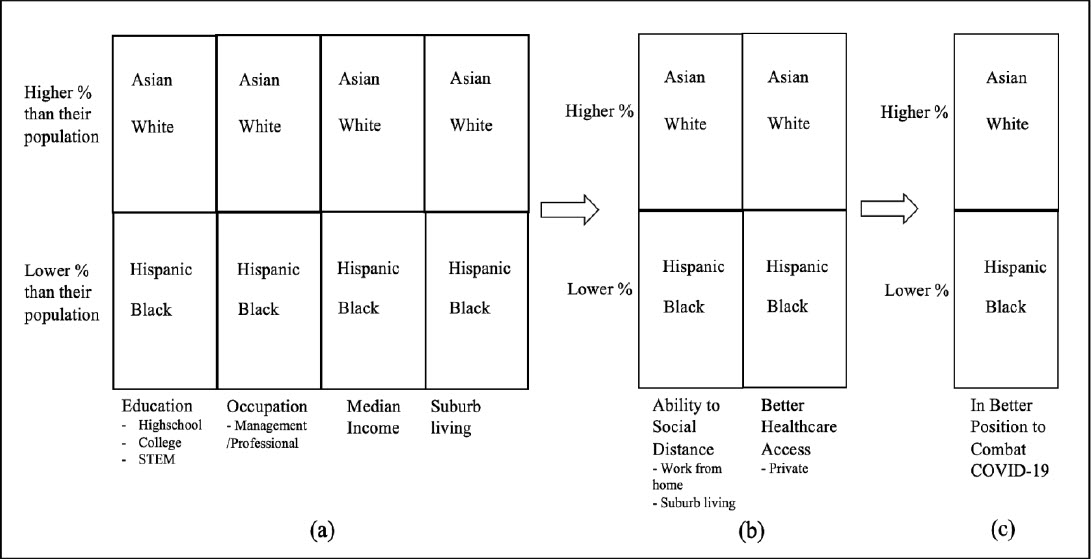
Figure 9: Race/ethnicity based socio-economic implications for COVID-19Considering QLCH7, Asians and Whites with higher proportions of Management/professional jobs instead of Service jobs (including essential work of hospitals/transportation/farm/grocery stores jobs) do have better capacity to social distance by living in non-crowded neighborhoods like suburbs instead of cities while the opposite is applicable to Blacks and Hispanics.
Utilizing QLCH8, Asians and Whites with higher proportions living in non-crowded neighborhoods, such as more suburban areas, have better healthcare access compared to Blacks and Hispanics. Figure 9 summarizes race/ethnicity based socio-economic implications for COVID-19. In Figure 9(a) Asians and Whites in relation to Hispanics and Blacks have higher percentages in education including STEM degrees which leads to higher percentages in Management/professional jobs instead of Service/essential jobs, thus additionally leading to higher median incomes. Higher median incomes for these two races give them the choice of living in more suburban areas. This allows higher percentage of Asians and Whites, in comparison with Hispanics and Blacks, the ability to social distance by living in suburbs as well as working from home (i.e. being of Management/professional occupation instead of being Service/essential workers as shown Figure 9(b)). This leads to Asians and Whites being better positioned to combat COVID-19 as displayed in Figure 9(c).- Comparison of regression analyses with socio-economic analysis
Our two regression analyses summarized in Table 2 and Table 4 showed that where you live (state) and race are statistically significant with COVID-19 deaths for the US population. These quantitative regression analyses are in concert with our QLCH based analyses conclusions for both race/ethnicity and where you live described in Figure 9. Tables 5 through 9 support these conclusions for the US population.
- Comparison of regression analyses with socio-economic analysis
- Conclusions
In the United States, deaths caused by infectious diseases have significantly reduced over the last 40 years due to better vaccines, therapeutics, and healthcare system improvements. However, in the first eight months of 2020, infectious disease has once again become a significant cause of death in the US. COVID-19 caused deaths have already exceeded the 170,000 deaths due to accidents in 2017. Unfortunately, this year COVID-19 caused deaths will be the third leading cause of deaths behind heart disease and cancer. Demographic factors of age groups, race, and residence state were found to be statistically significant using multiple regression analysis. The second analysis, with factors of age groups, gender, and residence state had a better R-squared adjusted score and no outliers. The virus is an equal opportunist as it affects both genders equally. However, the age of an individual is a critical variable that decides life or death, especially for individuals in age groups of 55 and above. Race also seems to play an important role in deaths, as Black and Hispanic death proportions are higher than their respective population proportions. Bigger population states with high minority populations have seen higher deaths relative to the other states. Thus, inequality in socio-economic conditions is an important determinant affecting health conditions of an individual and his/her ability to social distance at work or at home. Socio-economic analysis for the US population shows that QLCH of education, occupation, and income affects race differently. For a given race, education drives occupation then income, where a person lives, and in turn his/her access to healthcare coverage. Considering US socio-economic data in the QLCH framework, we conclude that different races are poised for differing effects of COVID-19. In particular, Asians and Whites are in a better position to combat COVID-19 when compared to Hispanics and Blacks.
- Competing Interests
The author declared that no conflict of interest exists in this publication.
How to Cite this Article:
Kulkarni, S. S., & Lorenz, K. E. (2020). Social Implications of COVID-19 Deaths: Analyzing Race, Ethnicity, Socio-Economic Conditions, Gender, and Age for the US. Advanced Journal of Social Science, 7(1), 163-180. https://doi.org/10.21467/ajss.7.1.163-180
References
[1] Heron M. National Vital Statistics Reports Volume 68, Number 6, June 24, 2019, Deaths: Leading Causes for 2017.
https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_06-508.pdf
[2] 2. el Bcheraoui C, Mokdad AH. Dwyer-Lindgren L., et al. Trends and Patterns of Differences in Infectious Disease Mortality Among US Counties, 1980-2014. JAMA. 2018;319(12):1248-1260. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5885870/
[3] Lee C. “Race” and “ethnicity” in biomedical research: How do scientists construct and explain differences in health? Soc Sci
Med. 2008; 68: 1183-1190. https://pubmed.ncbi.nlm.nih.gov/19185964/
[4] Pareek M, Bangash MN, Pareek N, et al. Ethnicity and COVID-19: an urgent public health research priority. The Lancet Volume 395, Issue 10234, P1421-1422, May 02, 2020. https://pubmed.ncbi.nlm.nih.gov/32330427/
[5] Rentsch CT, Kidwai-Khan F, Tate JP, et al. Covid-19 by Race and Ethnicity: A National Cohort Study of 6 Million United States Veterans. Preprint. medRxiv. 2020;2020.05.12.20099135. Published 2020 May 18.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7273292/
[6] Vahidy FS, Nicolas JC, Meeks JR et al. Racial and Ethnic Disparities in SARS-CoV-2 Pandemic: Analysis of a COVID-19 Observational Registry for a Diverse U.S. Metropolitan Population. medRxiv 2020.04.24.20073148;
https://www.medrxiv.org/content/10.1101/2020.04.24.20073148v2
[7] Millett GA, Jones AT, Benkeser D, et al. Assessing differential impacts of COVID-19 on black communities. Annals of Epidemiology, Volume 47, July 2020, Pages 37-44. https://www.sciencedirect.com/science/article/pii/S1047279720301769
[8] Centers for Disease Control and Prevention, Deaths involving coronavirus disease 2019 (COVID-19) by race and Hispanic origin group and age, by state. Accessed 20 August 2020. https://data.cdc.gov/NCHS/Deaths-involving-coronavirus-disease-2019-COVID-19/ks3g-spdg.
[9] Centers for Disease Control and Prevention, Provisional COVID-19 Death Counts by Sex, Age, and State. Accessed 20 August 2020. https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-S/9bhg-hcku
[10] de Brey C, Musu L, McFarland J, National Center for Education Statistics, U.S. Department of Education, NCES 2019-038. Status and Trends in the Education of Racial and Ethnic Groups 2018. Accessed 20 August 2020.
https://nces.ed.gov/pubs2019/2019038.pdf
[11] U.S. Bureau of Labor Statistics, Labor Force Statistics from the Current Population Survey HOUSEHOLD DATA
ANNUAL AVERAGES 11. Employed persons by detailed occupation, sex, race, and Hispanic or Latino ethnicity. Accessed 20 August 2020. https://www.bls.gov/cps/cpsaat11.pdf
[12] Berchick ER, Barnett JC, Upton RD. Health Insurance Coverage in the United States: 2018. Issued November 2019 P60-267(RV). Accessed 20 August 2020. https://www.census.gov/content/dam/Census/library/publications/2019/demo/p60-267.pdf
[13] Centers for Disease Control and Prevention, National Vital Statistics Reports Volume 68, Number 9 June 24, 2019 Deaths: Final Data for 2017. Accessed 20 August 2020. https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_09-508.pdf
[14] U.S. Census Bureau, Current Population Survey, 1968 to 2018 Annual Social and Economic Supplements. Real Median Household Income by Race and Hispanic Origin: 1967 to 2017. Accessed 20 August 2020.
https://www.census.gov/content/dam/Census/library/visualizations/2018/demo/p60-263/figure1.pdf